
Designing for Rural India — Part 1
Journey of designing OpenCHS with Samanvay
India does not have a National health insurance or universal health care system for all its citizens. This has propelled the private sector to its dominant position in the healthcare market. Private companies provide the lion’s share of healthcare services in the country.
Despite the structures in place to ensure equality and funding from government and non-government sources, we still observe a visible gap in access to healthcare in rural areas compared to cities. A staggering 68% of the population lives in rural areas and has no or limited access to hospitals and clinics. Consequently, the rural population mostly relies on alternative medicine and government programmes.
If one had to paint a picture of rural India, it would be people living in mud houses in small villages. These villages have next to no electricity supply. There are setups of solar power stations which people use to charge their cellphones. Travelling to these villages is not always easy. One would require to change at least three different modes of transport to reach many of these villages. The residents seek out healthcare in cases of pregnancy and severe illness like Tuberculosis, Dengue, etc. However, villagers often do not seek treatment for early symptoms which appear less dangerous. This is not always due to lack of awareness. It is often also the case that infrastructure to support the long tail of healthcare is simply not that accessible in rural India.
Healthcare in Rural India
The public healthcare in rural areas has been developed as a three-tier structure based on predetermined population norms.
1. CHC (Community Health Centres)
Community Health Centres form the uppermost tier and are established and maintained by the State Government. Community health centres are staffed by four medical professionals supported by twenty-one paramedical and other staff. Surgeons, physicians, gynaecologists and paediatricians provide comprehensive care in each CHC.
Each CHC has thirty indoor beds, an Operating Theatre, X-ray, Labour Room, and Laboratory facilities. The community health centre provides expert facilities in obstetric and other care for patients referred to them by the four primary health centres within their jurisdiction.
2. PHC (Primary Health Centres)
Primary Health Centres (PHCs) comprise the second tier in rural healthcare. PHCs provide integrated, curative and preventive healthcare to the rural population with emphasis on preventive and promotive aspects. Activities include promotion of better health and hygiene practices, tetanus inoculation of pregnant women, intake of IFA tablets and institutional deliveries. A medical officer is in charge of the PHC supported by fourteen paramedical and other staff. Each primary health centre has four to six beds. Patients are referred to the PHCs by six sub-centres.
3. Sub-centres
A sub-centre is the most peripheral institution and the first contact point between the primary healthcare system and the community. An Auxiliary Nurse Midwife (ANM) is in charge of six sub-centres each of which provides basic drugs for minor ailments. A sub-centre provides services in relation to maternal and child health, family welfare, nutrition, immunisation, diarrhoea control, and control of communicable diseases. ANMs also use Anmol Tablet, a product that aids in maintaining and collecting data, specific to primary health.
4. Non-government Infrastructures
Apart from the government bodies there are other players in the system, which are closest to the villagers (bottom most in this tier). There are private hospitals, which run to provide special services or even basic healthcare.
Accessing health support is not that easy for village residents. They have to travel long distances to visit public hospitals spending money, and time that could be spent doing their daily chores. That’s when community health services come to play.
There are non-profit NGO Hospitals which run Community Health Services (CHS). They hire and train health workers who work closely with villagers in providing health services and education.
Health Workers who work as a part of the Community Health Services are known as VHWs (Village Health Workers), as a part of CRHP (Comprehensive Rural Health Programme). Jamkhed is a programme run under CRHP.
Jamkhed is centered around mobilising and building the capacity of the community, empowering the people to bring about their own improvements in health and poverty-alleviation. This is one of the better known and appreciated community health systems.

Role of VHW ( Village Health Workers )
VHWs are individuals selected by the villagers. They are responsible for providing consultation and prescription on basic health care. Their appointment by the community helps establish villagers’ trust in them.
VHWs typically take care of a single village, but if required, they can be responsible for up to five villages. They are trained in basic healthcare, understanding symptoms and personality development. Since they are only trained in basic healthcare, they escalate severe cases and recommend the patients to visit hospitals. Quite often these volunteers are women.
Apart from this, VHWs also bust widely held superstitions by providing elementary health education.
Health workers use their considerable interpersonal communication skills to bring about important behavioural changes with respect to reproductive and hygiene practices in their rural communities.
How do they operate now?
The infrastructural support that these health workers get is mostly via Community Health programs and some inventory support from the government.

Here are some highlights about their daily operations -
Use of Paper:
The health workers still use paper for most of their work. They are provided with a chart that maps various symptoms to common ailments and relevant medication. While this may enable the health workers to swiftly treat common ailments, the strict mapping unfortunately severely restricts their ability to correctly identify edge cases or more subtle health issues.
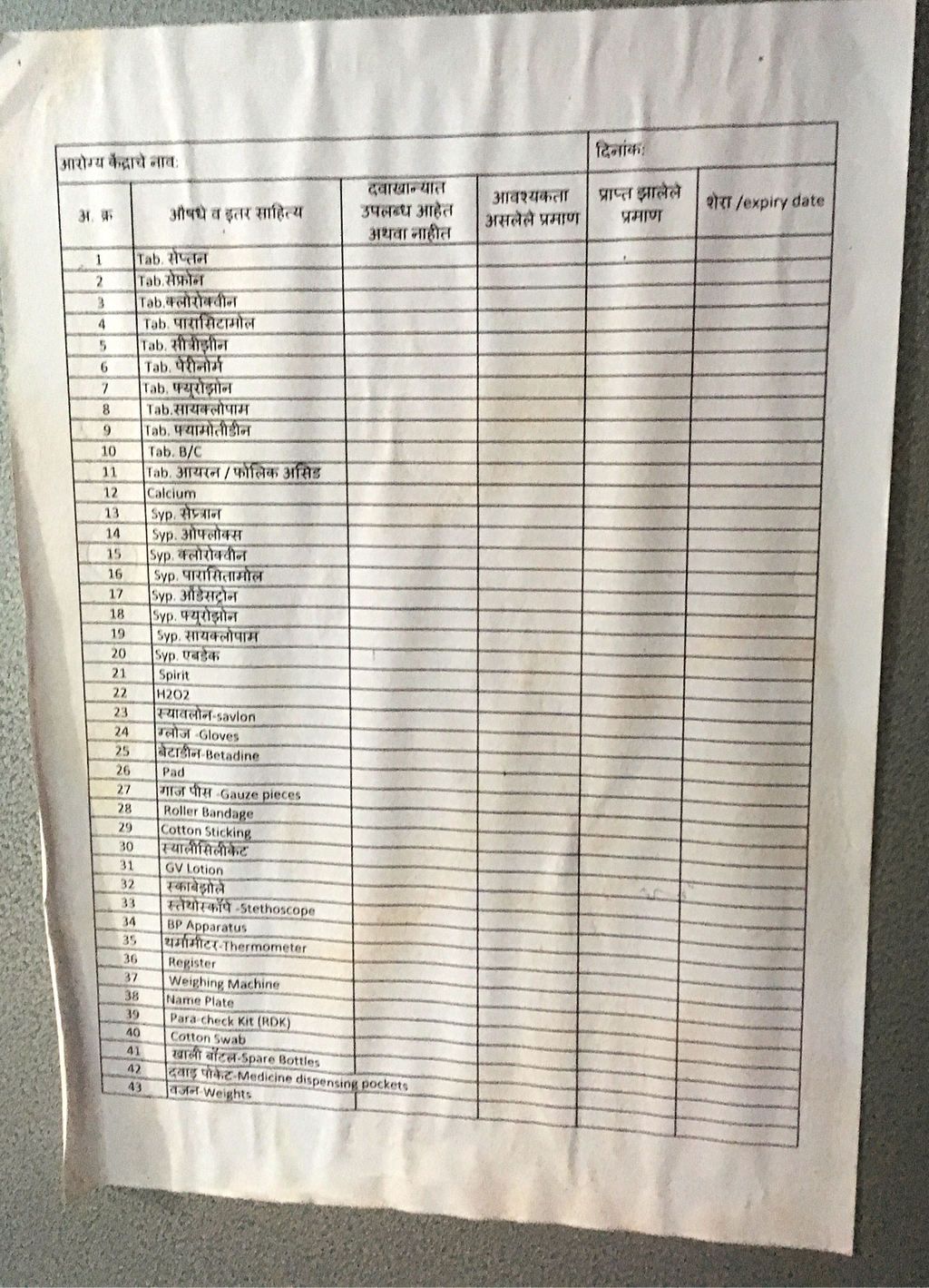
Inventory List:
Procurement of medicines is also done using paper. Health workers also track the need for medicines, availability and expiry dates of the medicines. Medicines are procured from Sub-centres where the health workers visit often to give reports to ANM’s about their respective villages.
Patient History
The health workers aren’t equipped to look at patients history at the time of consultation. They keep manual records which are too comprehensive to look into at the time of visits.

How does OpenCHS help?
OpenCHS strives to fill this gap and provide a decision support system that helps a health worker perform diagnoses. The system also provides the health workers with the steps for treatment.
What is OpenCHS?
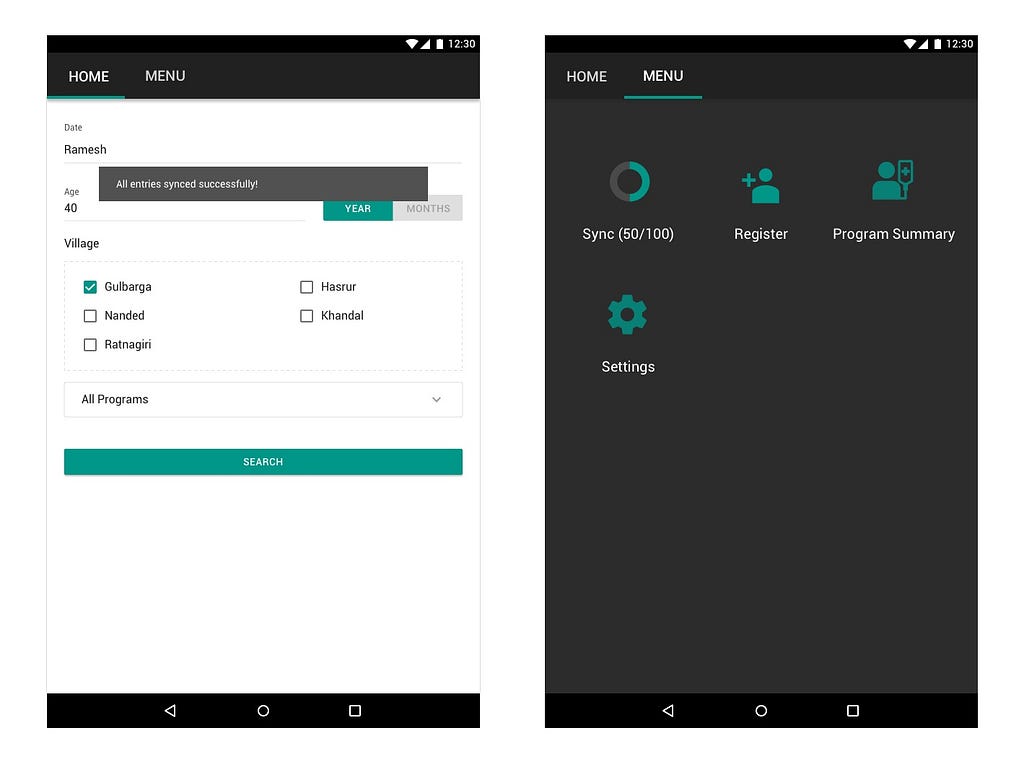
OpenCHS is an Open Community Health Service platform that works in collaboration with NGO Hospitals. OpenCHS is a mobile app that is used by Village Health Workers (VHW) in the field or in their clinics when patients visit them.
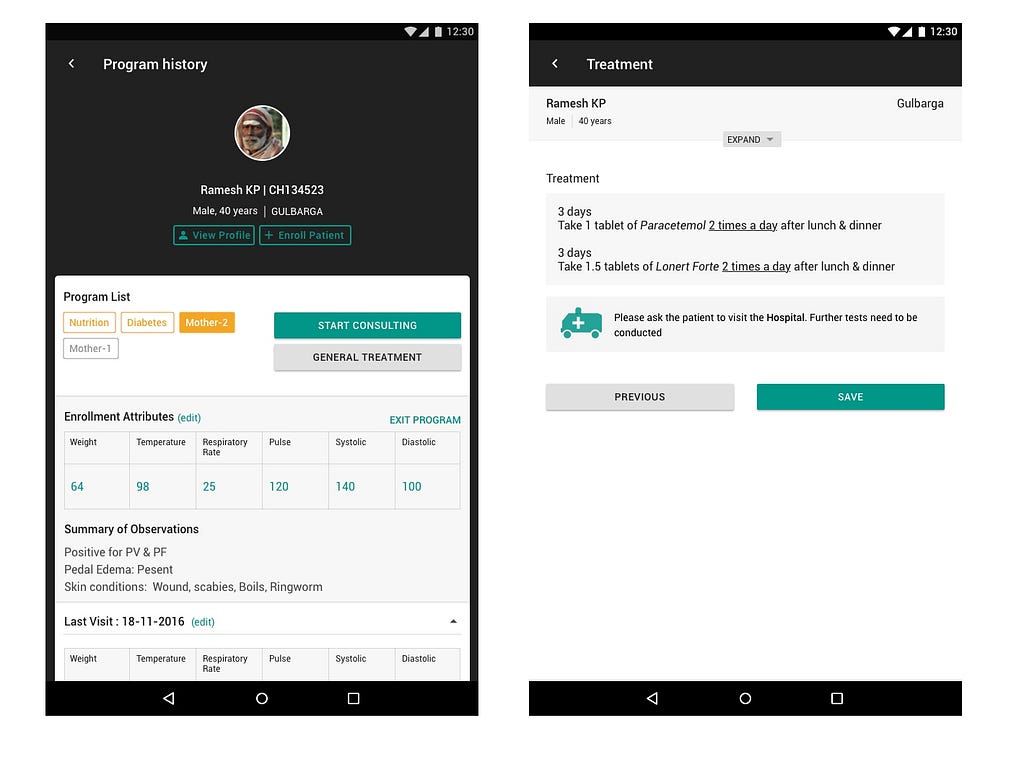
OpenCHS helps VHWs to record patient data, perform diagnoses and manage programme statuses. The app also enables the health workers to consider individual patients’ medical histories during their diagnoses.
Our challenges while designing the product
- Physical Constraints: Data is not recorded as someone on a desk job would. Health workers not only collect data with the app but they also have to use health equipment to take measurements. This requires the health workers to keep switching their attention between the patient and the application.
- No Electricity and Network Connectivity: VHWs don’t have access to electricity. They use basic cellphones (not smartphones), which they charge using solar charging stations located at central areas of villages. There is also next to no network connectivity which makes it difficult for an application to work in the field.
- Localisation & Multi-lingual Support: The application is intended to be used throughout multiple states of India. Each state has their own language. Some villages within a state may even use multiple dialects. We focused on providing multi-lingual support and localisation, in particular with regard to specialised medical terminology and concepts.
- Ease of Use: VHWs live in remote villages of India, where there is very little or no access to technology. They are used to basic cellphones, i.e. no smartphones. We had to be cautious about not having a higher learning curve for the application for them, so they don’t face issues when they are in the field.
What did we do?
Considering the challenges and constraints that we were working with, this is how we approached the design of the application.
It works offline:
We were aware that the user is not going to be connected to a network 98% of the time, so we made the app work offline. We store all data locally on the device. The app only connects to a server when synchonising data. Typically health workers visit a sub-centre or another place with internet connectivity monthly. Recorded data is reported to the hospitals as part of the synchronisation.
Decision Support:
The application provides decision support based on the recorded data and suggests treatment. We built our algorithm in collaboration with medical practitioners and took into account common health procedures. The algorithm even helps the health worker identify emergencies and provide appropriate medical care. When a patient needs medical attention from a trained medical professional, the application suggests them to inform the patients of the details and visit a hospital.
Localisation and Multi-lingual Support:
The application will be implemented with multi-lingual support. For each implementation, there will be localisation for specialised medical terminology used by the residents of the villages. Currently, we have an implementation in Marathi, which can be downloaded from here.
Ease of Use:
Ease of use was our major focus while designing this application.
- Keep it simple, focused: We tried to understand different activities that a Health Worker performs, and based on those use cases, created focus in the application, instead of going by one interface for all flows, like a dashboard.
- Attention on Iconography: We experimented with iconography using various styles and even with contextual icons. This quickly proved infeasible given that our users were stretched through rural India.
We followed these simple rules of iconography:
- Keep it simple and schematic, i.e. avoid details
- 5 second rule, if you can’t think of that icon in five seconds then that icon probably is not a good choice
- Memorability, making the icons distinct enough that they are remembered even after prolonged usage.
- Understand Behaviour: We tested an alpha version of the application with Health Workers to see if they are comfortable with data entry and understand input fields as concepts. To our surprise, the first thing the health worker did was swipe on the screen. It was most interesting because we knew that our users don’t use smart phones, so how did this come up as a first interaction in this person’s head? Perhaps media has been reaching them through means which one can’t imagine.

So, What’s next?
The application is yet to be released. The plan is to implement it at one village first and then scale accordingly.
We are looking forward to two types of feedback. After the implementation of the application, the health workers will be trained. At this stage will be able to get quick feedback about usability and other challenges.
The second feedback will have a rather longer loop, where the health workers will be using it in the field and on their return we will learn about how it went and get more qualitative feedback. Here is all the documentation, including designs of the project so far.
Want to know more?
There has been much discussion about each flow and decision, in multiple small and large sessions that we will be sharing in detail shortly so that you can better understand our efforts. Keep on the lookout :)
Thanks to nilenso and Samanvay team for the opportunity to work on this interesting problem. I also appreciate the feedback from Kenneth & Trouble in better articulating this post.
Do get in touch with me (noopur@nilenso.com) for any further questions or details. Any feedback will be highly appreciated.

Noopur wrote this story to share knowledge and to help nurture the design community. All articles published on uxdesign.cc follow that same philosophy.

Designing for Rural India — Part 1 was originally published in UX Collective on Medium, where people are continuing the conversation by highlighting and responding to this story.
